
Tickborne Disease Highlight: Tularemia
|
Figure 1:
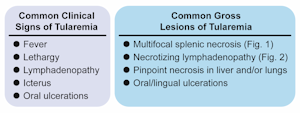
Common clinical signs and gross lesions of tularemia. |
|
|
Figure 2:
Multifocal to coalescing splenic necrosis |

|
|
Figure 3:
Cut section of enlarged & necrotic lymph nodes. |

|
By Drs. Kelli Almes and Megan Niederwerder
Warmer weather has arrived and so have the infectious diseases and vectors that go along with it. In the Midwest, especially Kansas, that means ticks and tickborne diseases in both humans and our pets. Two of these diseases that all too often have fatal consequences for our feline patients are Francisella tularensis, the causative bacterium of tularemia or rabbit fever, and Cytauxzoon felis, the causative parasite of cytauxzoonosis or bobcat fever. Tularemia can also have serious, and occasionally fatal, consequences in humans. F. tularensis is highly infectious with only a few organisms needed for transmission, which can occur via aerosolization, ingestion, or through the bite of an infected tick. A correct and rapid diagnosis facilitates proper treatment with appropriate antibiotic therapy.
The tick vectors that transmit tularemia are all present in Kansas and are capable of transmitting other zoonotic agents1 (Table 1). F. tularensis is transmitted to cats by the infected tick feeding on the cat or the cat ingesting the infected tick, typically during grooming. Cats can also become infected from feeding on an infected rabbit carcass, being bitten or scratched by another infected animal, or through mechanical transmission from other blood feeding insects. The incubation period is approximately 3-5 days. Common clinical signs and gross lesions are listed in Figure 1 and images are shown in Figures 2 and 3. Many of these same clinical signs can be seen with Cytauxzoonosis; these two pathogens must be differentiated to initiate proper treatment and safety precautions.
Antemortem testing can be challenging, but submission of a lymph node aspirate from an enlarged node for bacterial culture at KSVDL can yield a diagnosis. The aspirate should be collected sterilely and placed in a preservative free tube. Proper personal protective equipment, including gloves and eye protection, is recommended while performing this procedure. Lymph node biopsy could also yield a definitive diagnosis but requires anesthesia and significantly more stress on the patient. If animals have died from a suspected infection with F. tularensis, we recommend submitting the entire animal for necropsy, ancillary testing, and proper disposal. This provides the best chance of a definitive diagnosis and reduces the exposure risks for the attending veterinarian and their staff. We do not recommend performing an in-clinic necropsy for sample collection.
Francisella tularensis is a select agent due to its potential to pose a severe threat to both human and animal health. Select agents are maintained on a federal list and specific regulations have been set for working with and disposing of these organisms. All cases of tularemia submitted to KSVDL are confirmed by the CDC and potentially contaminated tissues are rendered sterile by autoclave on site. If a cat is suspected of having tularemia, the necropsy will be performed in a biosafety cabinet to prevent aerosolization of the bacteria and minimize any potential exposure.
If an animal is diagnosed with tularemia, the owner or any other human with potential exposure should seek advice and possible treatment with their physician. The oral lesions present in many of these cats readily transmit the bacteria and thus, a history of saliva contact or biting should be thoroughly investigated.
References:
1Tickborne Diseases of the United States (https://www.cdc.gov/ticks/diseases/index.html)
|
Table 1. Tickborne diseases and tick vectors |
|||
|
Tick Species and Common Name |
|||
|
Amblyomma americanum
Lone Star tick |
Dermacentor andersoni
Mountain Wood tick |
Dermacentor variabilis
American Dog tick |
|
| Francisella tularensis | X | X | X |
| Heartland Virus | Suspected | ||
| Rocky Mountain Spotted Fever | X | X | |
| Ehrlichiosis | X | ||
| Colorado tick fever | X | ||
KSVDL Welcomes Dr. Douglas Marthaler to the Diagnostic Team
Return to Index