
Johne’s Disease Outbreak in a Beef Herd
Drs. Jamie Henningson and Gregg Hanzlicek
Background: Johne’s disease is the clinical manifestation of an infection of Mycobacterium avium subspecies paratuberculosis (MAP). Infection occurs typically in young calves less than 6 months of age.1 The source of infection includes, in-utero transmission, colostrum, milk, and fecal-oral routes. In cow-calf operations, fecal-oral is the most common route of transmission. Although infection occurs at an early age, the clinical signs of this disease are not observed until animals become adults (median age 5 years), and the incidence of clinical disease is usually sporadic.2 This case is unusual because several adults were reported to have begun showing clinical signs within a few days of each other.
History: A cow-calf producer reported 4 adult crossbred cows in herd of 85 cows dying over the course of two weeks (two within the same day). All other herdmates, including both cows and calves, appeared to be healthy during this same time period. The herd had purchased multiple cows through a salebarn over the previous 5 years.
Clinical signs: Over the course of one week and several months earlier all 4 cows had developed chronic diarrhea immediately after calving. No other clinical signs were observed, and the producer reported the affected animals’ appetites and attitudes to have been normal. The cows were treated multiple times with internal parasiticides and a variety of antibiotics and probiotics (without veterinarian recommendations).
Diagnostics: Necropsy in combination with histopathology and the identification of the agent in lesions is the gold standard test for diagnosing Johne’s disease. A necropsy was performed on the last 2 cows by the local practitioner and tissues were submitted to KSVDL. The body condition for both was recorded as 2 (scale 1-9). Submandibular edema was also noted in one of the animals. In both cows, portions of the intestine were thickened with a “corrugated” appearance suggestive of late-stage MAP infection (Figure 1). No other abnormalities were observed grossly. Histopathology revealed granulomatous inflammation in the intestinal wall (figure 2); a special stain was positive for acid-fast bacilli confirmed Johne’s disease in both cows.
Outcome: After the necropsy results were reported, a representative group of adult animals were sampled and ELISA was completed to assess the prevalence of Johne’s in this herd. Test results indicated the within-herd prevalence was 24%. A site visit was conducted and a Johne’s Risk Assessment was performed by KSVDL veterinarians in cooperation with the local practitioner. Several environmental and management areas of potential sources of exposure to high levels of MAP were identified. Considering the estimated Johne’s prevalence in this herd and the producer’s long term goals, a Johne’s disease prevention plan was devised and included: 1) calving and feeding in a manner that would minimize the exposure of young calves to adult manure, 2) annually testing adult animals every year before calving, 3) purchasing replacements from herds with known Johne’s prevalence (not the local salebarn).
Take home messages: The more common Johne’s disease temporal pattern includes sporadic, single animals and not clusters as in this case. This case indicates that sometimes multiple animals (at least 2 in this case) can become clinical within a narrow time frame; therefore, when multiple animals present with chronic diarrhea and weight loss, Johne’s should be on the ruleout list. Other take home messages include the importance of knowing the source of replacement animals and testing adults before entry to the herd. This case also highlighted the importance of conducting a Johne’s Risk assessment to establish management practices that help minimize the spread of this disease in cow-calf herds.
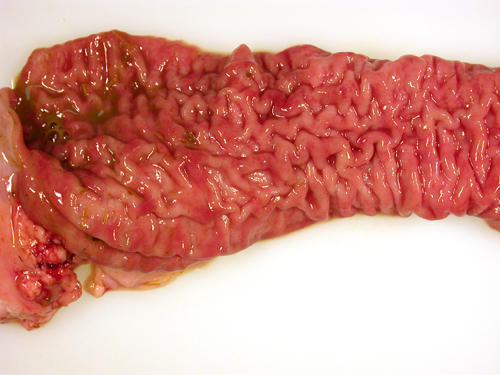 | 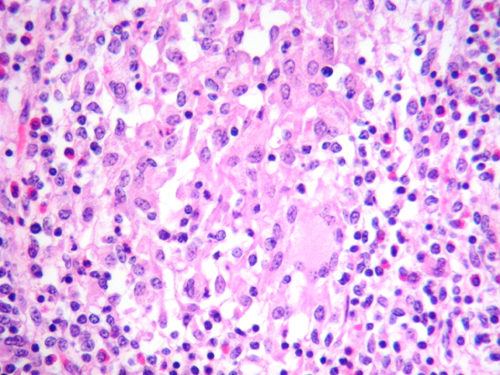 |
Figure 1. | Figure 2. |
References:
1. Johne’s Information Center. http://www.johnes.org/
2. Michael T. Collins, School of Veterinary Medicine, University of Wisconsin-Madison. http://www.merckvetmanual.com/generalized-conditions/paratuberculosis/overview-of-paratuberculosis
